Gastrointestinal (GI) bleeding is among the most common gastrointestinal disorders and can range from microscopic bleeding to massive bleeding leading to hypovolemia and shock. In children, GI bleeding requires prompt assessment, diagnosis, and treatment. Two issues should be addressed immediately: the child’s appearance, mental status, blood pressure and heart rate, and the likelihood of ongoing bleeding. It is important to determine whether the bleeding is from an upper or lower GI source because this will help in the diagnosis and treatment.
GI bleeding may have different clinical presentations ranging from hematemesis or hematochezia with or without hemodynamic instability, to melena or rectal bleeding. Hematemesis refers to the vomiting of fresh red blood or coffee-ground material from lesions in the esophagus, stomach or proximal bowel. Blood losses are often more marked in upper than in lower GI bleeding. Hematochezia (red blood passed per rectum) usually indicates a lower GI source and usually in the colon. Melena (black, tarry, foul-smelling stool) usually indicates an upper intestinal source. Occult bleeding, a positive stool guaiac, is usually found after clinical manifestation of chronic blood loss. Patients may have chronic GI bleeding with asymptomatic iron-deficiency anemia, or hemoccult-positive stool on evaluation of children with gastro intestinal problems.
Accounting for 10-15% of referrals to pediatric gastroenterologists, GI bleeding can be categorized by location as well as broken down into age groups. In neonates, the most common upper GI bleeding is from swallowed maternal blood. Rectal blood should be tested for fetal hemoglobin to rule out maternal blood. Stress gastritis is found mainly in neonates in intensive care and highly correlated with prematurity, neonatal distress, and mechanical ventilation. Hemorrhagic disease of the newborn is caused by a deficiency in vitamin K and has nearly disappeared since the introduction of routine vitamin K administration shortly after birth.
In infants and children, esophagitis is the most common cause of upper GI bleeding caused by severe gastroesophageal reflux, and is present in infants with regurgitation, dysphagia, and failure to thrive. Children may present with bleeding as a result of ulcerating or erosive esophagitis. Other causes include mechanical injury from a foreign body, chemical injury, or medication and infection. Gastritis is often associated to Helicobacter pylori infection. Other causes are from nonsteroidal anti-inflammatory drug use, Zollinger-Ellison syndrome, inflammatory bowel disease, and esophageal and gastric varices secondary to portal hypertension. Peptic ulcer disease is most common in children older than one year and is the most common cause of hematemesis. Trauma can be a cause of bleeding in rare cases.
Anorectal fissures are the most common cause of lower GI bleeding in neonates and children. When associated with constipation, they respond well to stool softeners and lubricants. Necrotizing enterocolitis (NEC) is common in premature infants. Symptoms of this condition include abdominal distension, poor feeding, vomiting, diarrhea, frank or occult bloody stools, lethargy and apneas. Newborns who have malrotation with midgut volovulus or proximal outlet obstruction typically present with abdominal distension, billous emesis, and melena. Malrotation is life threatening and requires emergent evaluation and treatment. A limited upper gastrointestinal contrast series is the best examination to visualize the duodenum.
Intussusception is the most common cause of intestinal obstruction in infants between 6 and 36 months of age. Approximately 60% of children are younger than 1 year, and 80% are younger than 2 years old. Symptoms include severe abdominal pain, which causes them to be irritable and draw up their legs. They may vomit and pass bloody stools and then improve for a while before the cycle repeats. When it is suspected, an emergency surgery referral is important. Milk or soy-induced colitis is an inflammatory enteropathy caused by ingestion of milk or soy proteins, and occurs almost exclusively in infants. Up to 25 % of patients with cow’s milk protein intolerance will have a cross-reaction to soy protein. Treatment involves eliminating the protein from the diet if the infant is breastfeeding, or the use of casein-hydrolysate formula.
Meckel’s diverticulum is the most important source of small bowel hemorrhage in children. It is present in 2% of the population less than 2 years old. Diagnosis is by radionuclide scan or surgical exploration. Beyond infancy, juvenile polyps are the most common source of significant rectal bleeding. Children present with painless bleeding per rectum, which often streaks the stool with fresh blood. Sometimes the patient will report prolapse of a mass from the rectum.Infectious diarrhea and inflammatory bowel disease (ulcerative colitis and crohn’s disease) can cause significant GI bleeding. Bleeding may be less common in crohn’s disease, but both may consist of bloody diarrhea, which can lead to acute or persistent bleeding resulting in anemia.
Recent antibiotic use raises suspicion for antibiotic associated colitis and clostridium difficile colitis. Vascular lesions consist of a variety of malformations that include hemangiomas, arteriovenous malformations, and vasculitis. These can lead to bleeding making localizing the bleeding practically difficult.
Many things children eat can look like blood. Red food coloring found in foods like Jell-O or Kool Aid, as well as fruit juices and beets may resemble blood, if vomited. Melena may be confused with dark or black stool from iron supplementation, bismuth subsalicylate, dark chocolate, grape juice, spinach, cranberries, or blueberries. A simple Hematest performed at the bedside can confirm presence of blood in gastric contents or in stools. In the neonate, the Apt test will differentiate maternal from infant blood.
An upper or lower endoscopy can be used to evaluate GI bleeding and is the procedure of choice for a diagnosis; and sometimes used in emergency cases. Where endoscopy is non-diagnostic, a bleeding scan, Mickel’s Diverticulum Scan, Capsule Endoscopy or Angiogram can be used.
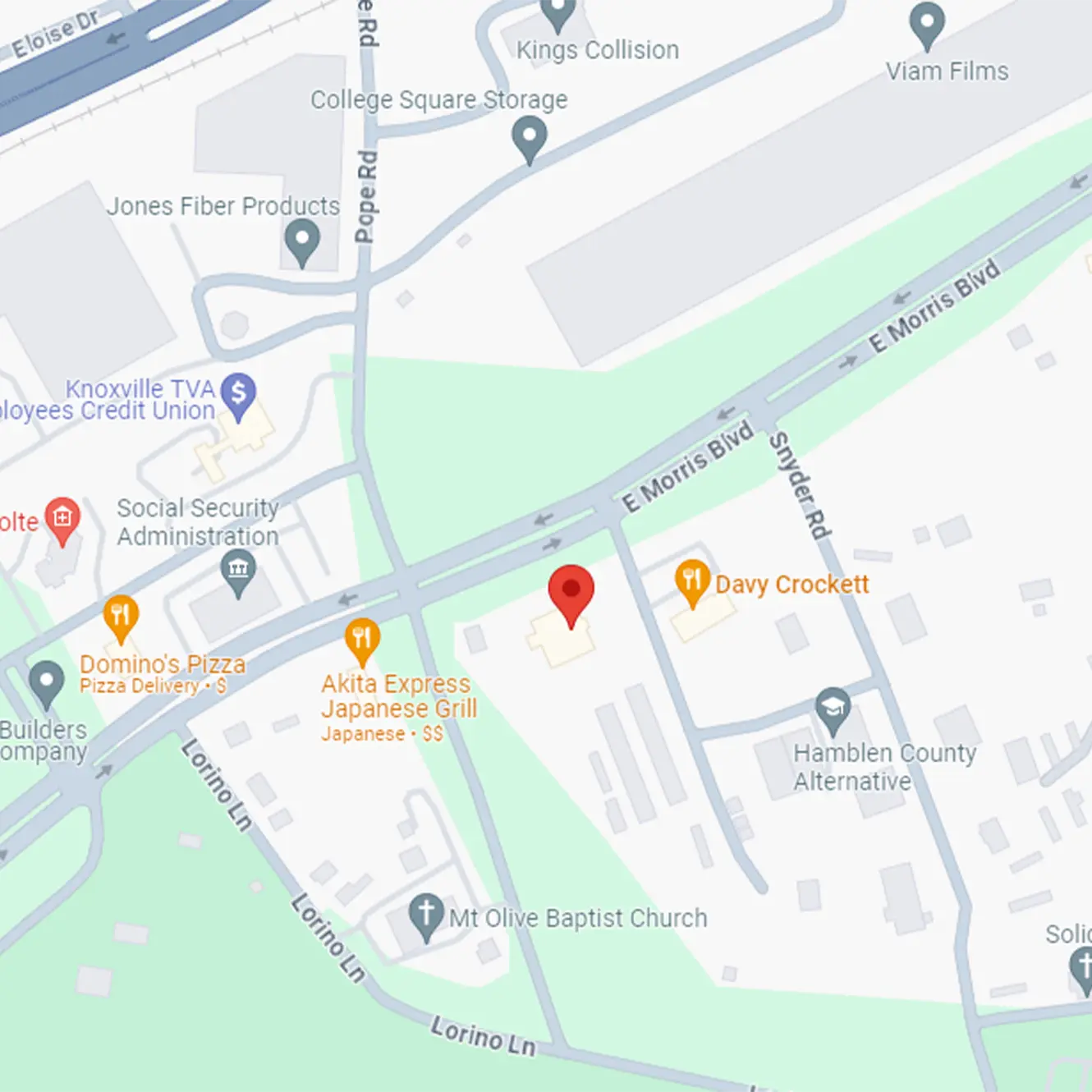
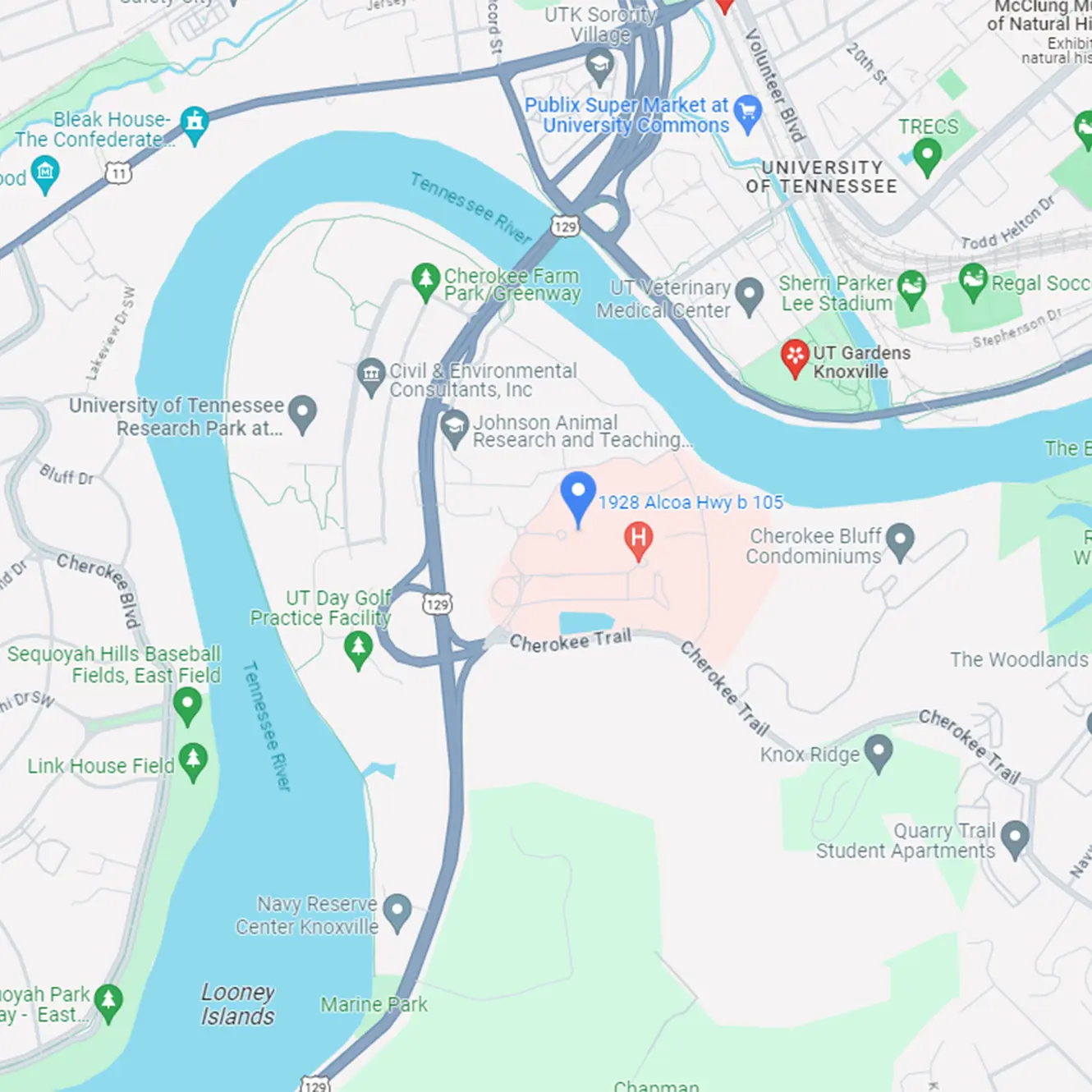
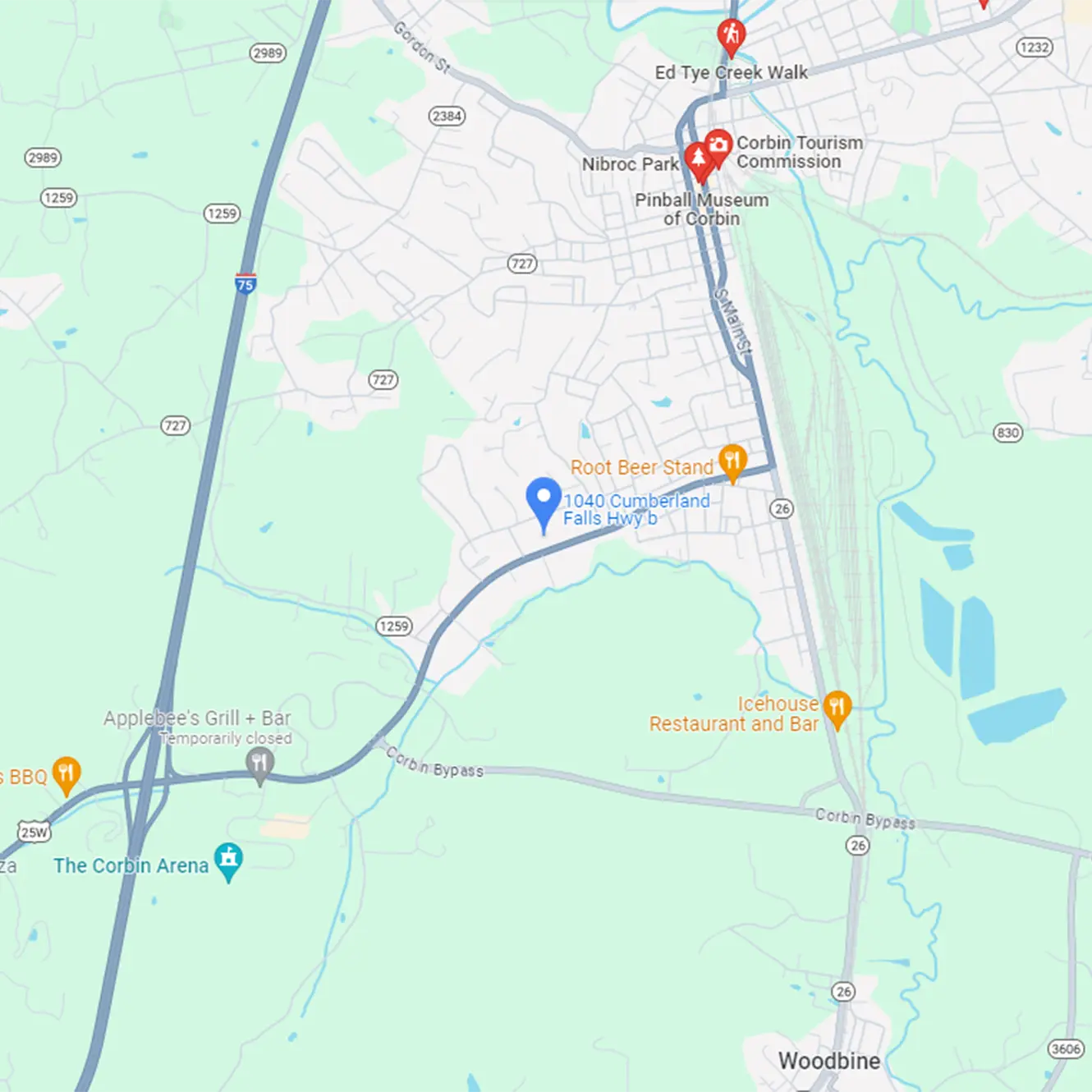
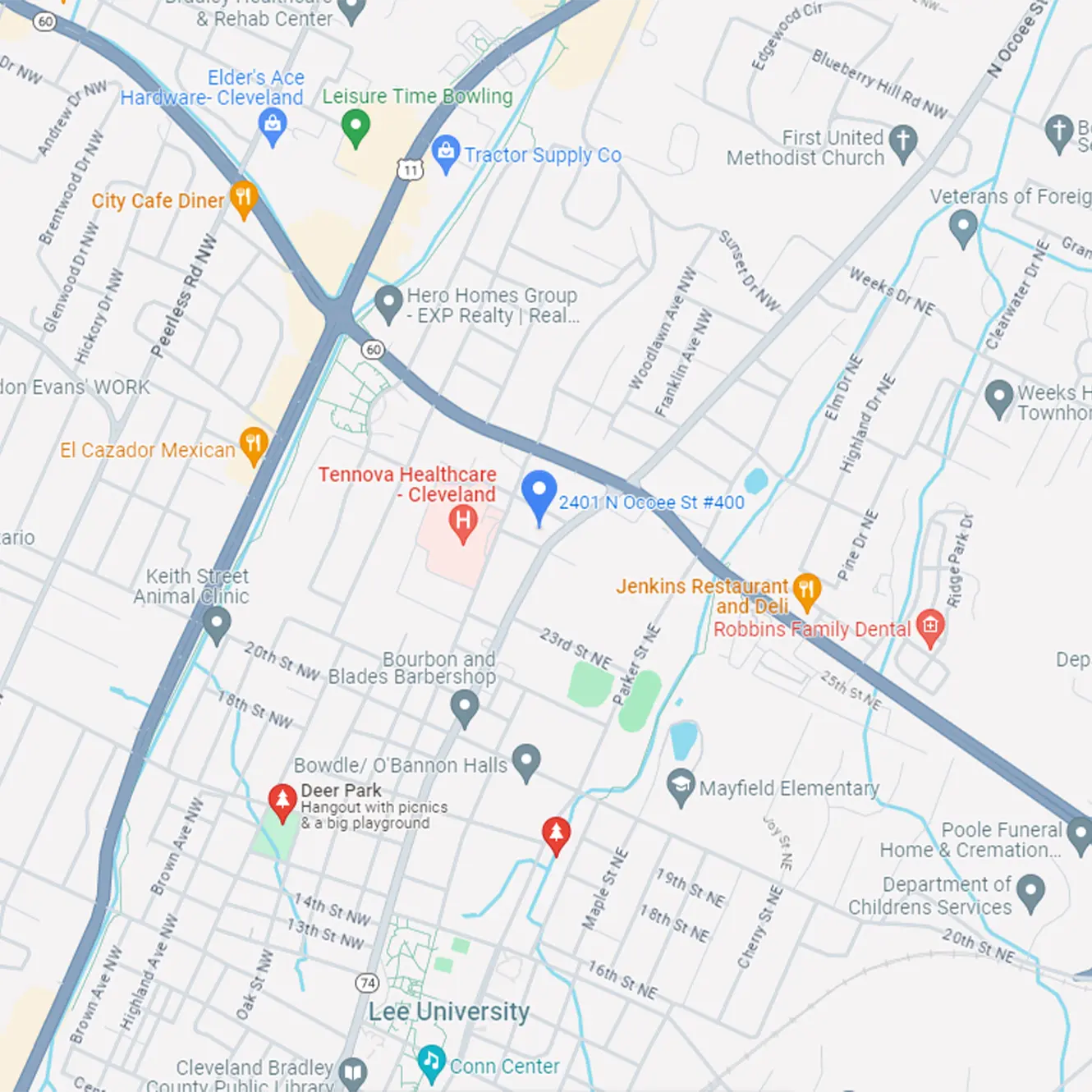
At East Tennessee Children’s Hospital, we have a state of the art endoscopy suite supported by multiple pediatric specialists that include surgeons, anesthesiologists, intensive care specialists, radiologists, hematologists, and other specialists on call, as needed, to help our team manage and care for these patients. If you have any patients or questions about your patient, please do not hesitate to call (865) 546-3998. For more information on our testing and services, please refer to our website: www. GIforkids.com