Gastroparesis refers to a condition where the muscles of the stomach work poorly or not at all. The stomach’s muscles are supposed to contract so food can go through the digestive system. The food is not ground up enough and doesn’t empty into the intestine the way it should. This prevents the food from being digested correctly and can cause nausea and vomiting and problems with blood sugar levels and nutrition.
Causes
There are many health problems that cause gastroparesis. Gastroparesis may be caused by problems with the brain’s ability to communicate with nerves in the gastrointestinal tract. This slows the contraction of the muscles in the intestines, which help to move food along. Gastroparesis may also result from congenital abnormalities, infection (viral infections), or systemic diseases (diabetes or autoimmune problems).
In addition, factors that may make a person more susceptible to developing gastroparesis include medications that can inhibit nerve signals (anticholinergics), renal disease, cystic fibrosis, and malnutrition.
Symptoms
The primary symptoms of gastroparesis are nausea and vomiting. Other symptoms include:
- Abdominal pain
- Bloating
- Feeling full quickly when eating
- Weight loss
- Heartburn
- Not wanting to eat (no appetite)
- Gastresophageal reflux
- Spasms in the stomach area
Diagnosis/Testing
Doctors use several tests to help diagnose gastroparesis and rule out conditions that have similar symptoms. Tests may include:
- Serological evaluation by taking a blood sample
- Upper Endoscopy (EGD) – is a procedure used to screen the upper digestive tract. A thin flexible tube with a -camera is inserted through the mouth into the stomach to evaluate your digestive system.
- Gastric Emptying Scan – Measures the time it takes for your stomach to empty.
- Motility studies – to diagnose your medical problem.
Treatment
The doctor may choose medications that act on nerve receptors such as cholinergic drugs or a medication that helps to empty the stomach such as metoclopramide Reglan . A surgical procedure may also be done that opens the area between the stomach and small intestine to allow food to flow more easily.
If gastroparesis is severe, and has not been helped by other methods, temporary feeding tubes or a G-J Tube Changes may be used to provide the body with needed nutrients. Total Parenteral Nutrition (TNP) may also be used to provide your body with nourishment.
Treatment also includes prevention of dehydration from continuous vomiting. Contact your doctor immediately or go to the Emergency Center if your child has the following signs of dehydration:
- Dry, sticky mouth No tears
- No urine in over 8 hours (or over 12 hours if child is more than 1 year old)
- Dark urine
- Child is unusually fussy or drowsy
- Child is extremely thirsty
- Child’s eyes look sunken
- Infant’s soft spot on top of head becomes sunken
Other signs that require taking your child to the Emergency Room immediately include:
- Fever over 103 degrees F (orally), or 104 degrees F (rectally)
- Severe stomach pain
- Blood in child’s stool or vomit
- Child’s poop is black
- Child’s vomit is green or black
- Child is difficult to wake up or seems confused
- Child will not drink
- Other symptoms that concern you as a parent
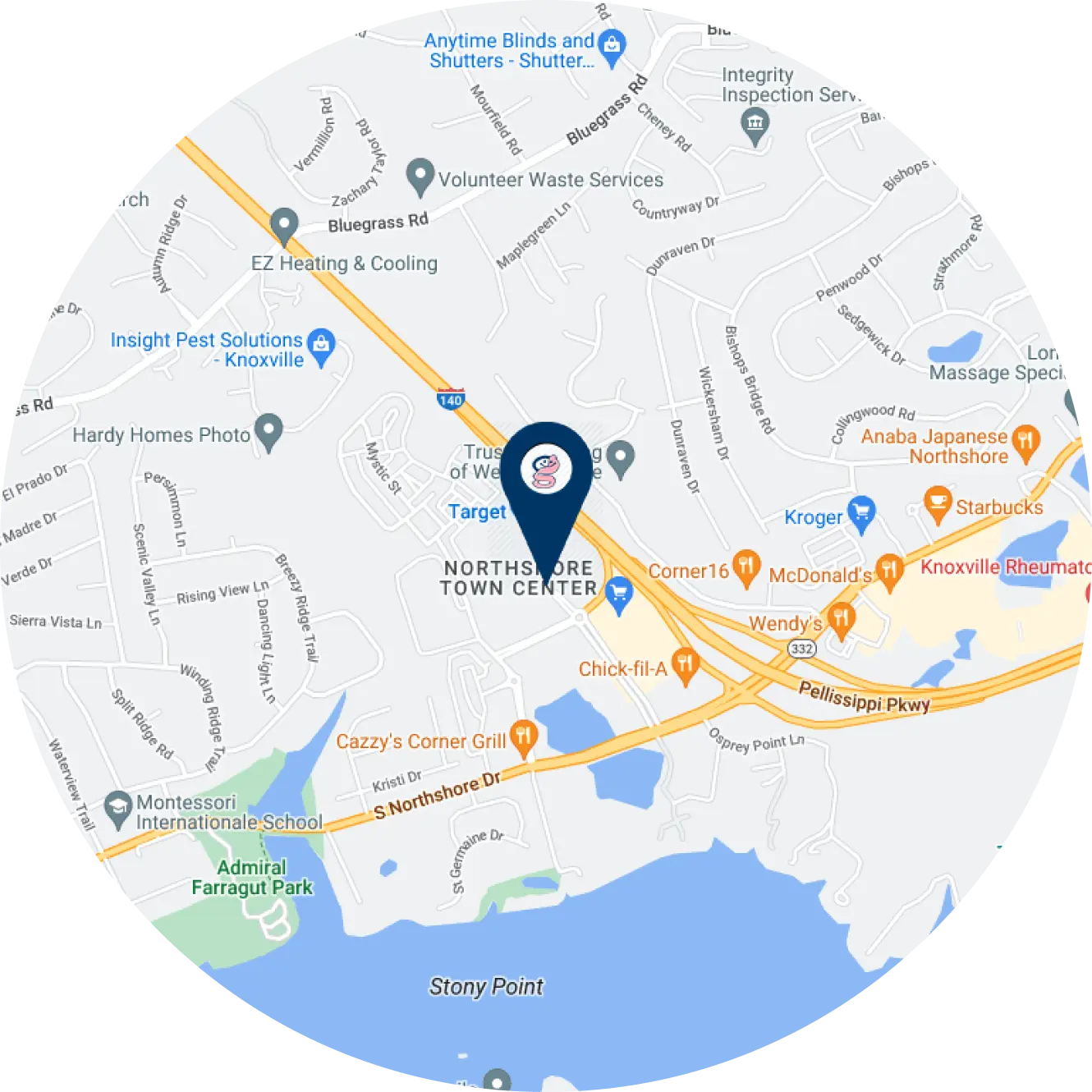
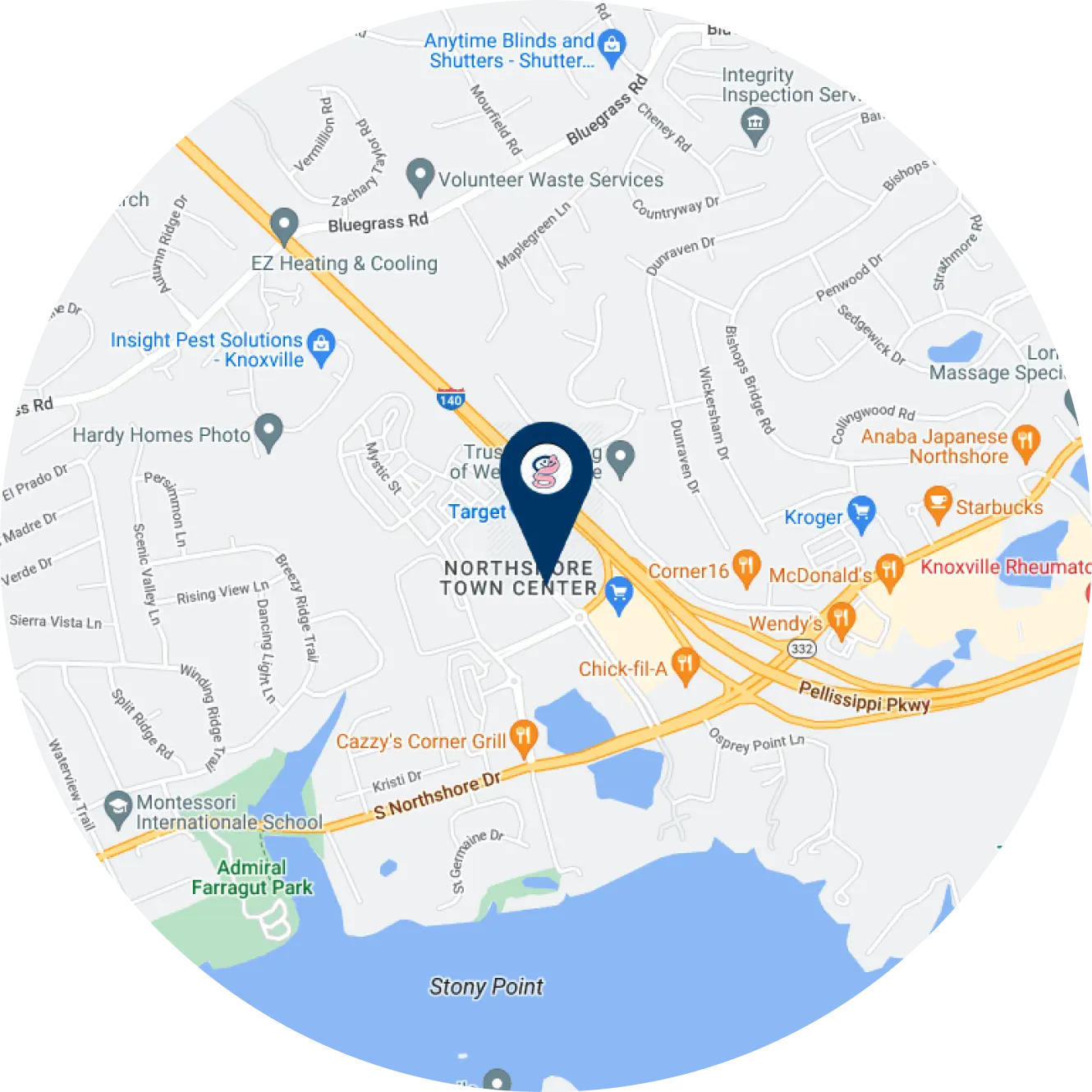
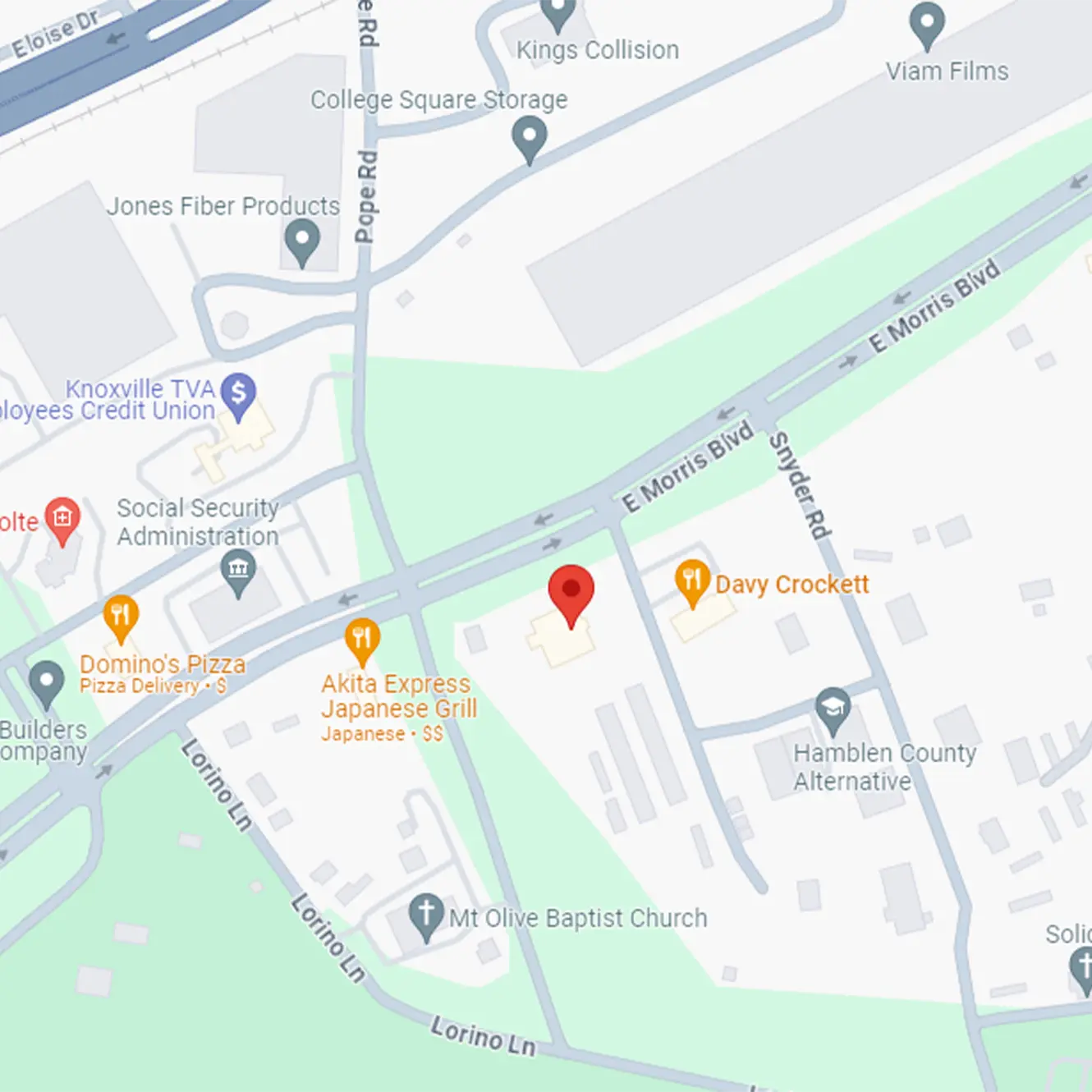
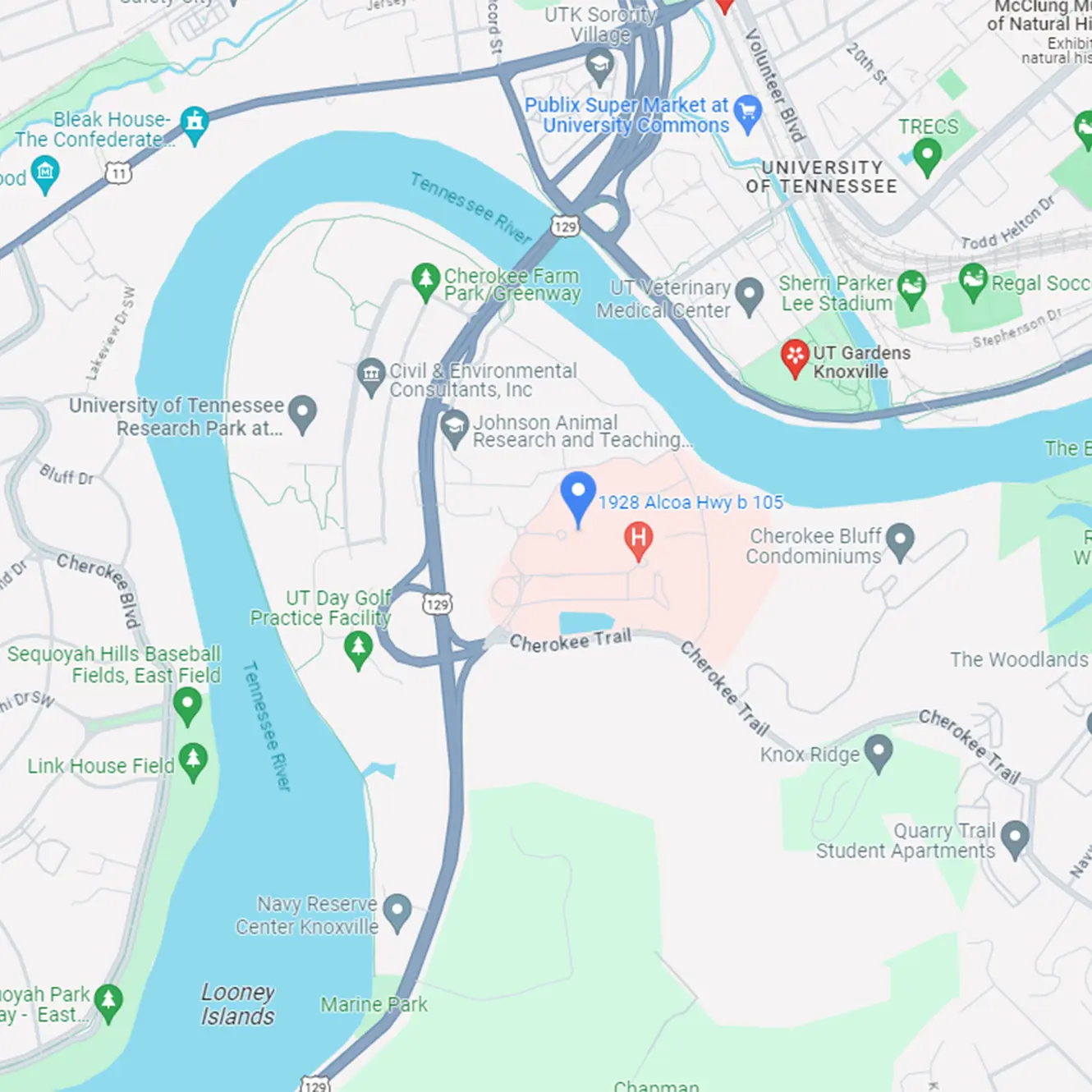
Dietary changes may be recommended to help control your symptoms. Consider meeting with one of our dieticians for a nutritional consult. Call (865) 546-3998 to schedule an appointment